Reversing COPD Progression And Lung Repair Support
Lung Anatomy And COPD:
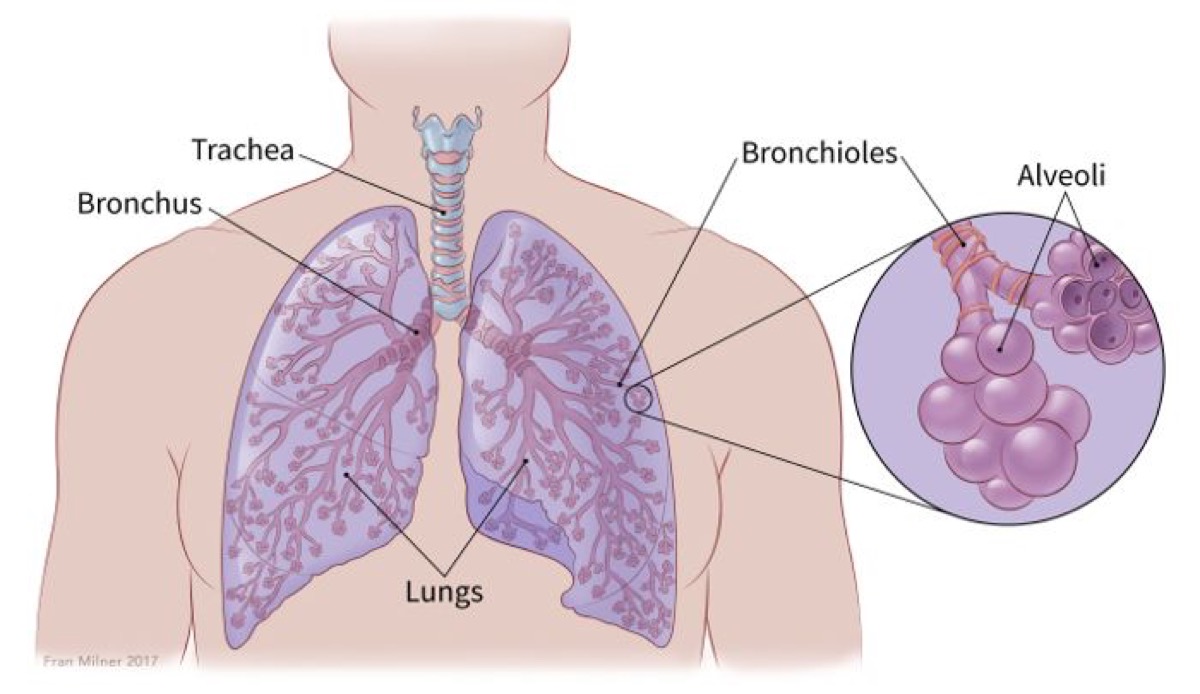
Before we talk about COPD, let’s briefly review our lung anatomy. There are two main parts in our respiratory system:
- Conducting zone: these are all large and small “pipes” that bring air into the lungs. They resemble an upside-down tree, starting with a large trunk (trachea) coming out from our throat, after which it divides first into 2 branches (left and right bronchi), and further 23 more times into smaller ones (bronchioles). [i] The tree’s “crown” is our lungs, which encase all of these structures.
- Respiratory zone: at the very bottom of all of those pipes there are 300 million little “bubbles” of air, called alveoli. These bubbles cluster together, resembling multiple grape vines. When we breathe in, these balloons fill with air and expand; when you exhale, they deflate. The walls of alveoli are lined with capillaries, through which alveoli release oxygen into the bloodstream, as we inhale, and absorb carbon dioxide from the blood, and breathe it out.
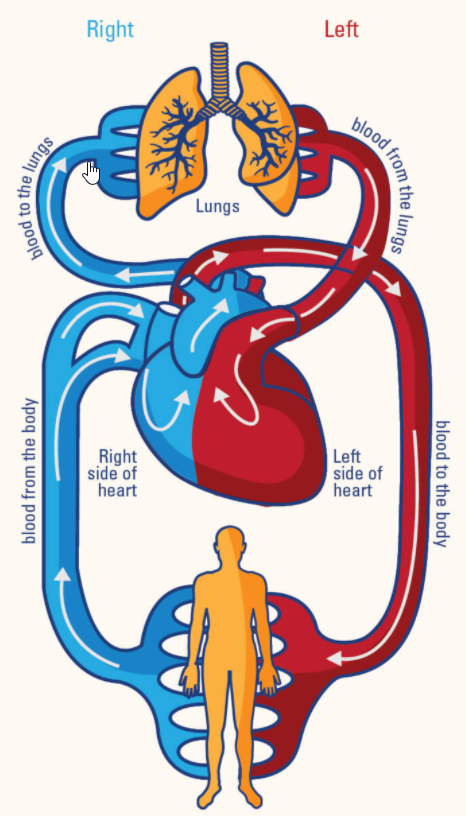
The Lungs and Other Organs
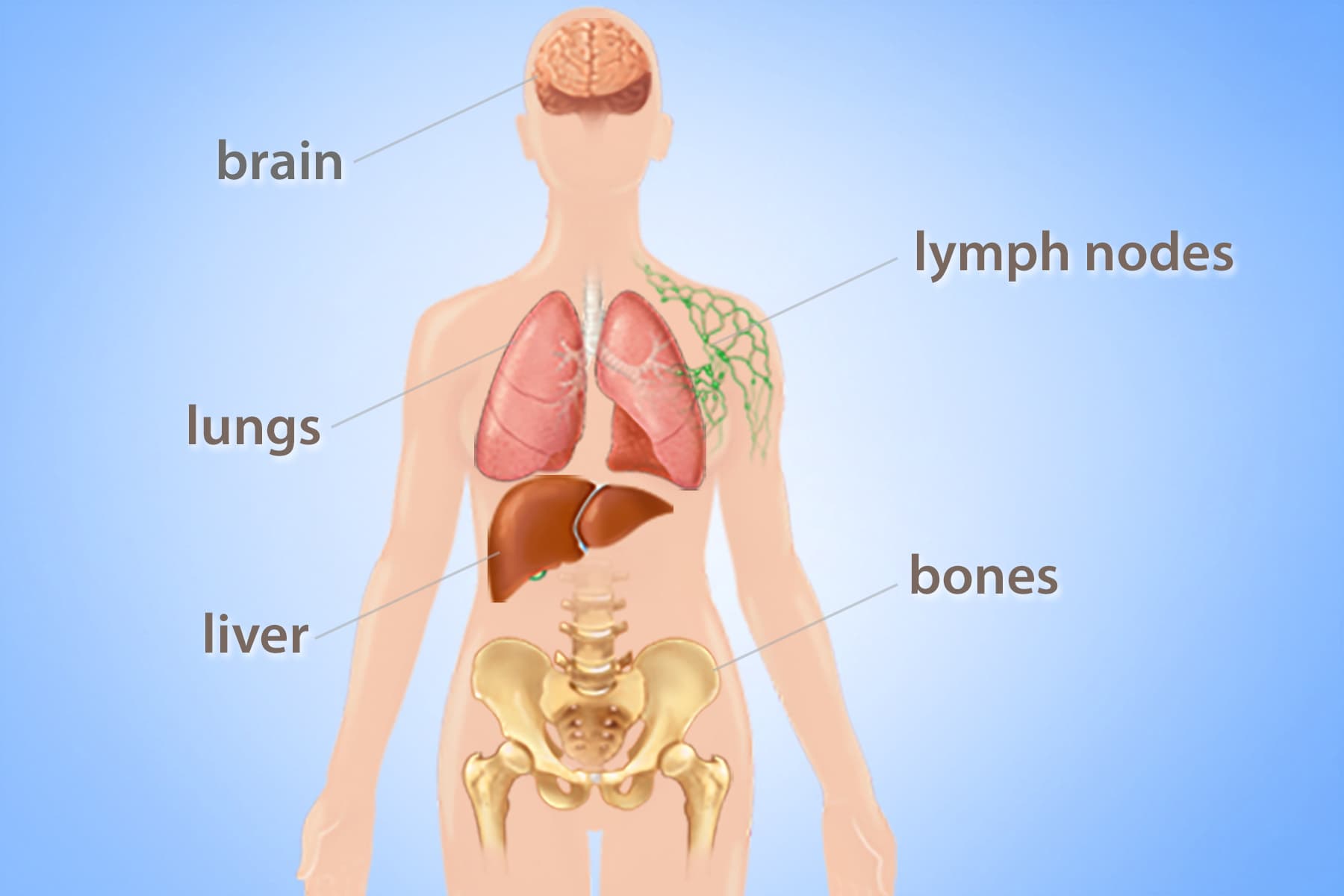
Lungs and heart are closely connected, as all blood coming from the lungs goes directly to the heart, from where it is pushed out to the rest of the organs. When the lungs do not function properly, it puts stress on the heart and may lead to heart enlargement and Pulminary Edema (swelling of the tissues, ex. ankles).
Lung and liver function are connected, too. Not only does oxygen gets released from alveoli into the blood, but also some toxic particles [ii] , which are carried to the liver for detoxification and elimination. When the liver is not working properly, the capillaries in the lungs become enlarged, and as a result, the red blood cells in them cannot absorb oxygen properly. [iii]
Lung and lymph are connected. Lymph vessels surround each alveolus. White blood cells called macrophages gobble up toxic particles. If the lymphatic system is sluggish, the person will be prone to chronic infections in the sinuses or ears, and/or acne in the upper body.
The lungs and brain are connected. The brain receives 25% of all oxygen we inhale. If the lungs are not working properly, a person may experience mental confusion, fatigue and other symptoms. And vice versa, a stroke may induce Pulmonary Edema (water in the lungs). [iv]
What is COPD?
COPD(Chronic Obstructive Pulmonary Disorder) is a lung condition that is frequent among smokers.
It is an airway blockage, caused by:
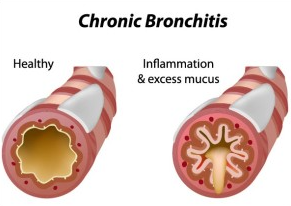
- Chronic bronchitis: Inflammation of bronchial tubes and accumulation of mucous.
- Symptoms: chronic cough lasting for many weeks or months, productive cough producing clear or white mucus (not green or yellow), wheezing or rhonchi, pressure or tightness in the chest, fatigue. When advanced, cyanosis (blue nails and extremities) and edema (water retention in extremities).
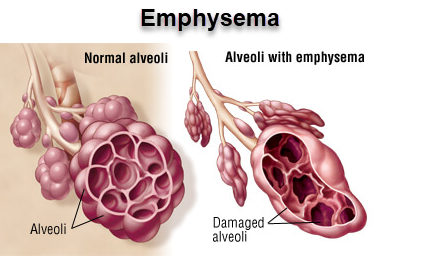
- Emphysema: damage to the small sacs in our lungs, called alveoli.
- Symptoms: severe dyspnea, and weight loss.
When alveoli break down, they become flat and hollow. Like a flat tire, these alveoli do not hold oxygen well. A combination of narrowing of the respiratory passage and damaged alveoli does not let the air exchange happen effectively, which causes breathing difficulties.
COPD Symptoms
COPD is characterized by:
| Symptom | Symptom Description | Caused by |
|---|---|---|
| Shortness of breath | when going up the stairs, or even after walking a short distance | inflammation of airways |
| Coughing up phlegm | sputum (saliva + mucous) in copious amounts, especially in the morning: white, yellow, clear, greenish in colour | excess mucous in lungs |
| Chronic cough | Cilia does not work well, body needs to help cough up mucous; most frequent in the morning | inflammation and swelling of airways |
| Wheezing | whistling sound during inhalation and exhalation | obstruction in the airways |
| Chest tightness | accompanied by painful deep breathing and making a person breathe shallow | infection in lungs |
| Blue lips and nails | occur in later stages of disease | lack of oxygen in the blood |
| Unintentional weight loss | Air isn’t released properly and gets trapped in the lungs. Chest expansion and breathing become difficult | increased work of breathing |
| Morning headaches | Accompanied by light-headedness and dizziness | Lack of oxygen |
| Sleeping issues | Especially uncomfortable in the morning, | Tightening of airways, becoming their smallest in diameter by morning |
| Extreme fatigue | Lack of stamina | Lack of oxygen, having to work harder to breather |
| Edema | Swelling in ankles | Stress on the heart due to lack of oxygen, poor blood circulation makes fluids pool |
| Chronic respiratory infections | Frequent colds, flu, pneumonia | Motility of lung villi is slower, and lungs cannot remove bacteria and viruses well |
Stages of COPD

In spite of the fact that many of us hear the word “COPD” and imagine people walking with an oxygen tank, this disease is much more common than people think. It starts so subtly, that most do not pay attention to its early symptoms. It is estimated that there are approximately 3 million Canadians suffering with COPD. [vi]
There are 3 stages of COPD:
- Stage 1 (Mild): 80% lung capacity – smoker’s cough, minor breathing difficulties, persistent cough with visible production of mucous. At this stage, symptoms are often attributed to other causes.
- Stage 2 (Moderate): 50-80% lung capacity – shortness of breath during light physical activity. Frequently people start taking at this point bronchodilators.
- Stage 3 (Advanced): 30-50% lung capacity – symptoms worsen, frequently flare up and last longer. At this stage, many people start taking steroids, and experience lung infections like bronchitis and pneumonia on a regular basis, and sometimes may require hospitalization, if their lungs get infected or exposed to highly-concentrated air pollutants.
What causes mucous [vii] excess in COPD?
Small amounts of mucous are produced in the respiratory passage by goblet cells every day. Its primary role is to moisturize and protect the airways. Mucous helps trap, move and protect the lining of respiratory pathways from toxins, bacteria and viruses that may enter during breathing.
Excessive mucous production starts where there is constant irritation of tissues by toxins. The reason body increases mucous when you smoke is because it tries to absorb copious amounts of toxins and prevent them from moving quickly, damaging tissues.
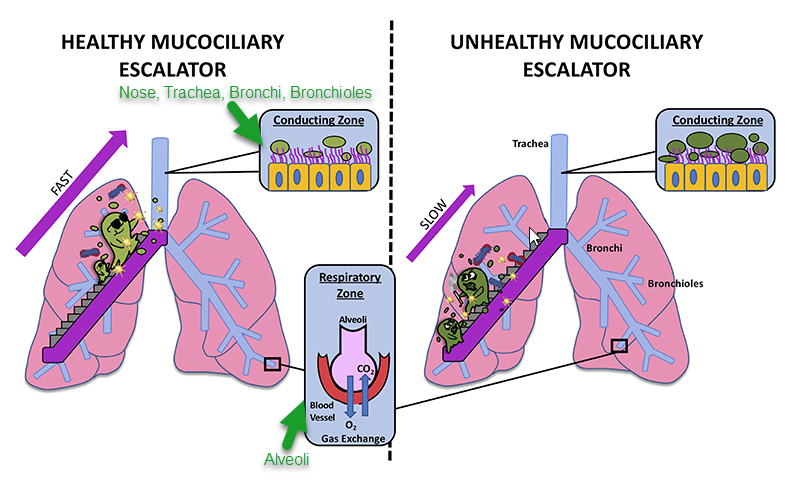
Mucous and Toxins Elimination in Lungs [viii]
The lung conducting zone, beginning from our nose, is covered with Celia, which are little, mucous-covered hairs, which move bacteria/viruses and debris up our throat with a speed of 900 beats per minute, as we inhale. If the lungs are strong and healthy, the trapped irritants will be expelled up the respiratory tract and either spitted or swallowed up.
Active aerobic exercises, such as running, tremendously help the body of a healthy person speed up the process of mucous elimination, which may be a great regular practice during COVID times. However, if the respiratory tract is in an extremely toxic state, a person may get sick when exercising, as the elimination of the toxins becomes above their liver’s capacity to neutralize them. You’ve heard about exercise-induced asthma or other similar disease symptoms.
Mucous Consistency and Celia Motility
Celia health is essential for the process to go smoothly. I the pictures below you’ll see 3 scenarios:
- Watery Mucous with healthy Celia: when the air quality is great, food is non-mucogenic (a plant-based diet with a high amount of raw foods) and the person is active.
- Thick and Viscous Mucous with healthy Celia: when the air quality is poor, food is mucogenic (high in animal and processed products), and the person is inactive.
- Damaged Celia with a moderate amount of mucous: after Celia is flattened or completely destroyed, it cannot move particles effectively, and those start accumulating in the lower portion of the respiratory tract. Severe damage of Celia is rare (hereditary, if a person inhales strong acids, cystic fibrosis, lung carcinoma).
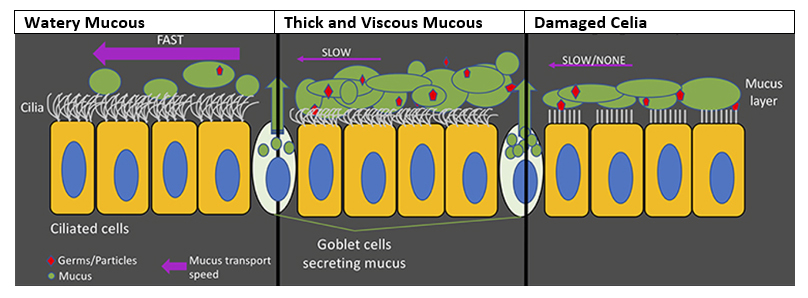
Some Celia impairment may occur due to heavy smoking and chronic inflammatory conditions, such as asthma, allergic rhinitis, chronic rhinitis and sinusitis. This issue is localized and may be reversible. [ix]
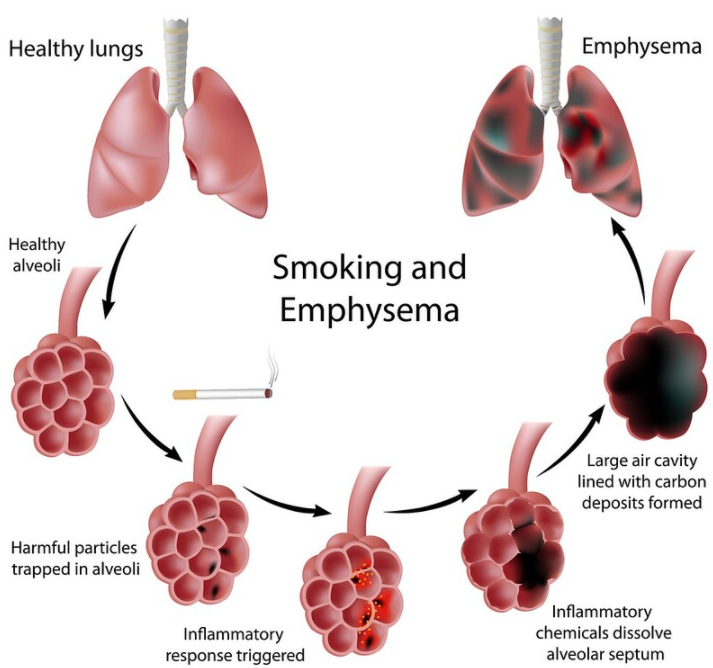
Complications of COPD
If toxins cannot be stopped in the conducting zone, they will start proceeding into the alveoli. The body will initiate inflammation, in order to mobilize white blood cells to destroy the toxins. However, in that process, partitions in the alveoli (called septum) get destroyed also. Carbon deposits form on the surface of alveoli, which further interferes with air exchange.

If you have COPD you are at increased risk of a number of complications [x] , including:
- chest infections – a common cold can easily lead to a severe infection
- pneumonia– a lung infection that targets the alveoli and bronchioles
- collapsed lung – the lung may develop an air pocket. If the air pocket bursts during a coughing fit, the lung will deflate
- heart problems – the heart must work extremely hard to pump blood through the damaged lungs
- osteoporosis – where bones become thin and break more easily. Steroid use in people with COPD is thought to contribute to osteoporosis
- anxiety and depression – breathlessness or the fear of breathlessness can often lead to feelings of anxiety and depression
- hypoxemia – caused by lack of oxygen to the brain. Symptoms include cognitive difficulties such as confusion, memory lapses and depression
- sedentary lifestyle – as symptoms of COPD progress, many people adjust their lifestyle to avoid symptoms. For example, they reduce their physical activity to avoid breathlessness. As they reduce their physical activity, they become less fit and even more breathless on exertion. This downward spiral of inactivity means they are prone to a range of potentially serious health problems, such as obesity and cardiovascular disease.
- tracheal, bronchial or lung cancer. Symptoms of lung cancer are coughing blood, chest and bone pain, unintentional weight loss, and a cough that does not go away. Respiratory cancer signifies that the tissue has been atrophying and “rotting” beyond the body’s ability to cleanse and repair it.
How Fresh Start May Help If You Suffer With COPD:

Here’s how we help you reverse the progression of COPD and provide lung repair support:
Quit Smoking Support: If you still haven’t quit, just do it!!! We’ll help.
Organ Screen: Upon arrival, we’ll do testing of your major organs of elimination, in order to see if any of them are especially struggling and needs support (liver, lungs, kidneys, large intestine, skin). We will provide that organ with the needed support.
Lung Cleanse and Therapies: it is impossible to start the healing of the lungs if they are overwhelmed with mucous and toxins. We use a steam bath, cold water treatments, halotherapy (cocoon) and other remedies to help your body remove irritants from the lungs.
Liver and Digestive System Cleanse: In order to cleanse lungs safely and effectively, you need to prepare other systems of elimination. This is exactly what we do via various methods of cleansing these organs.
Mucous Removal: The lymph system is responsible for the removal of excess mucous in our body, yet frequently works ineffectively. Using advanced lymph flush, deep breathing and exercise will help.
Skin Detoxification: See your skin becoming pink and healthy looking, vs grey and mottled.
Aromatherapy Massages and other relaxation therapies: Relaxation is an essential component in lung healing because this organ is related to our nervous system and brain function.
Healing Inflammation and Lung Restoration: we use various green juices, drink anti-inflammatory meals, and nourish and assist in the cellular restoration of your respiratory system. Most people see a major improvement in their cough, ability to breathe and a result, quality of sleep.
Emotional Wellness: Emotional wellness is connected to our lung health. During your stay, you’ll be able to work with our experienced emotional wellness specialists.
Disclaimer:
Though many of our guests receive wonderful results, the Fresh Start does not guarantee health recovery from any specific disease or symptom, or degree of its improvement, as the healing process is individual, gradual, multi-layered and depends on many factors. Please be realistic in expectations as there is no such thing as quick fixes when it comes to healing.
References:
[i] Eating Alive II. Dr. John Matsen, ND. p. 550. Goodwin Books, Ltd. 2004
[iii] What is Hepatopulmonary Syndrome. HPS Canada
[iv]Neurogenic Pulmonary Edema. Medscape. 2020
[v] Most Common Signs of COPD by Kathrine George. ActiveBeat. March 6, 2019
[vi] Quick facts about COPD. PROOF Centre of Excellence.
[vii] COPD.net. Increase in mucus and change in color. April 2, 2015
[viii] Moving Mucus Matters for Lung Health. Frontiers for Young Minds. September 11, 2019
[x] Lung conditions – chronic obstructive pulmonary disease (COPD). Better Health Channel